A revolutionary breakthrough in mitochondrial research has provided critical insights into the development of type 2 diabetes, paving the way for potential new treatments that target the disease at its root cause.
The findings, published in Science by researchers at the University of Michigan, reveal how dysfunctional mitochondria—often referred to as the “powerhouses of the cell”—directly impact insulin production and metabolic health.
Mitochondrial Dysfunction and Diabetes Progression
This pioneering research demonstrated that damaged mitochondria trigger stress responses within cells, affecting their ability to function properly. Specifically, the study found that mitochondrial dysfunction disrupts beta-cell maturation, which in turn impairs insulin production—a key factor in the development of diabetes.
Dr. Emily M. Walker, lead researcher of the study, stated:
“We’ve identified crucial pathways that maintain mitochondrial function, filling a major gap in our understanding of diabetes progression. This could fundamentally change how we approach treatment.”
A Systematic Approach to Mitochondrial Research
The research team examined three key areas of mitochondrial function:
✔️ Mitochondrial DNA integrity
✔️ Cellular pathways that eliminate damaged mitochondria
✔️ Mechanisms that maintain healthy mitochondria pools within cells
Their comprehensive approach revealed that disruptions in these processes could signal the nucleus to alter cell fate, particularly in insulin-producing beta cells.
A Universal Mechanism for Metabolic Disorders?
Dr. Scott A. Soleimanpour, director of the Michigan Diabetes Research Center, emphasized the broader significance of the findings:
“What makes this research so groundbreaking is its universal application. We identified the exact same stress response across multiple cell types, suggesting a common mechanism underlying metabolic diseases.
These discoveries could extend beyond diabetes, potentially providing new therapeutic targets for metabolic disorders and age-related diseases, where mitochondrial dysfunction is a known contributor.
A Breakthrough in Potential Treatments
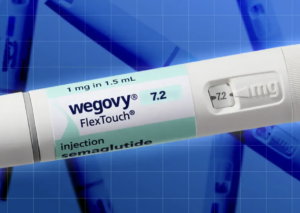
One of the study’s most promising findings was the identification of a drug, ISRIB, which was able to reverse mitochondrial damage and restore normal cell function.
Key Finding: After four weeks of ISRIB treatment, insulin-producing beta cells regained their ability to control glucose levels in diabetic mice.
“The ability to potentially reverse mitochondrial damage represents a paradigm shift in diabetes treatment,” Dr. Walker explained. “We’re not just managing symptoms; we’re addressing the root cause of cellular dysfunction.”
Expanding the Research for Clinical Applications
Encouraged by their success in pre-clinical trials, researchers are now conducting follow-up studies to replicate their results in human cell samples from diabetic patients.
Key Areas of Further Investigation:
How mitochondrial dysfunction affects multiple body systems during diabetes progression
The role of mitochondria in weight regulation, liver function, and muscle performance
Optimising ISRIB and related compounds for potential clinical use
A New Era for Diabetes Treatment?
Industry experts believe this breakthrough could lead to more effective treatments within the next decade. By targeting mitochondrial function, scientists may be able to develop novel therapies that go beyond symptom management—potentially reversing some of the damage caused by diabetes.
As research progresses, the scientific community remains hopeful that this new understanding of mitochondrial dysfunction could reshape the future of diabetes care.